enzyme histochemistry
Introduced in the 1960s by Raekallio, time-dependant changes in the activity of various enzymes at wound edges were evaluated, predominantly in experimental animals. The diagnostic value of these extrapolations has been questioned, however, as positive findings do not occur as consistently in humans as they do in experimental animals (Betz 2003).
immunohistochemistry
The detection of fibrin was thought to be proof of vitality, but can be deposited at the site of injury up to 6 hours after death. The morphological features of 'post mortem fibrin' are difficult to interpret.
Researchers have examined the relationship between cell-adhesion molecules (including the selectins P-selectin and E-selectin, as well as ICAM-1) and wound vitality. P-selectin positivity is increased in vital wounds, with strong staining visible in endothelial cells after a few minutes, and remains visible for up to 7 hours. Positivity for E-selectin is seen after 1 hour (up to 17 days).
Fibronectin (involved in leucocyte migration) immunohistochemistry, and evaluation of proliferation markers (such as Ki-67) and apoptoses have also been evaluated in the recent past.
Articles reviewing immunohistochemical parameters for wound age estimation;
- Betz (1995)
- Takamiya M et al (2002)
- Akasaka Y et al (2004)
- Suarez-Penaranda et al (2002)
- Kondo et al (2002a)
- Kondo et al (2002b)
- Fiegulth A et al (1997)
- Tarran et al (2006)(burns)
- Cecchi R (2010)
practical evaluation
Betz (2003) provides a useful summary of how to approach wound age estimation, given the vast amont of data available, much of which is based on experimental wound infliction, often on animals;
- the detection of fibronectin and interstitial collagens (with network-like structures distant from the wound margins and bleeding zone) is significant;
- the collagen response must be associated with fibroblast proliferation;
- negative and positive controls must be provided;
- multiple specimens from each wound need to be evaluated if a 'negative' finding is being relied upon.
Cecchi (2010) advises that the forensic pathologist should 'select the most appropriate markers' to be identified, according to the technology available in his/ her institute as well as the 'estimated timing' of the inflicted injury. For example, if it is thought that the wound is of the order of 2-3 hours, markers of endothelial activation might be appropriate (ICAM-1 and VCAM-1). Wound vitality markers of interest are those which apparently are 'never' or 'constitutionally scarsely' present (in human skin) such as Selectin-E and IL-1B, or are 'known to be absent' in post mortem wounds such as Fibrin D-dimer and Cathepsin A and D.
Future fields of research are likely to extend into the proteogenomics/ geno-proteomics of the inflammatory response, and Cecchi (2010) identifies NFkB activation as a key marker of interest.
histological changes
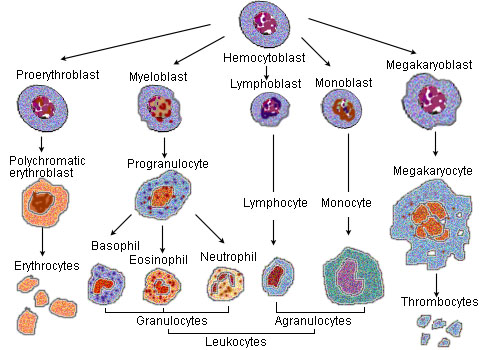
source: wikimedia
polymorph neutrophils
Although the presence of neutrophils is assumed to represent a vital reaction, it should be noted that they can reach damaged tissue passively, and only their presence beyond the bleeding zone should be regarded as positive evidence of migration. Similarly, margination of neutrophils in vessels may be due to artefactual attachment, whilst permeation of vessel walls is assumed to be a vital process (Betz 2003).
- earliest vital neutrophil reaction - 15-30 mins post wound infliction;
- routinely described as appearing after 15 hours; and
- have been described several months after wound infliction.
Therefore one can only say that a wound without neutrophils indicates a post-infliction period of less than 15 hours.
macrophages
Migration of macrophages to the area of damage occurs at the same time as neutrophils, but their reduced motility delays their appearance.
- earliest detection - 3 hours post infliction;
- usually found 3 days+ after wounding;
- a macrophage excess over neutrophils occurs at the earliest 20 hours post injury and routinely after 11 days.
Lipophages (macrophages incorporating fat) and erythophages (macrophages incorporating red blood cells) can be seen 3 days post wounding.
Haemosiderin (formed during the degradation of haemoglobin) can be detected by the Perl's stain (Prussian Blue) after approximately 3 days post wounding (Betz 2003).
(See also McCausland and Dougherty (1978) for a study of the histological ageing of bruises in lambs and calves)
granulation tissue and re-epithelialisation
This can be detected approximately 3 days+ after wounding. Complete re-epithelialisation in surgical wounds takes at least 5 days, and is routinely found after 21 days.
estimation of wound vitality and 'age' of wound
Traumatic insults to the skin result in an acute inflammatory response, and researchers in forensic pathology have attempted to define the characteristics of a wound inflicted during life (a 'vital' injury) as opposed to one inflicted after death.
Hernandez-Cueto et al (2000) re-produce Legrand du Salle's 'schema' for the diagnosis of vital and post mortem wounds;
| Vital wounds | Post mortem wounds | |
| Wound edges |
|
|
| Surrounding tissues
|
|
|
| Inside the wound |
|
|
(Source: Adapted from Hernandez-Cueto et al (2000))
histological parameters in age estimation of human skin wounds (Betz 2003)
| Parameter | Earliest appearance | Routine appearance | Latest appearance |
| neutrophils | 15-30 min | >15 h | months |
| macrophages | 2-3 h | >3 days | months |
| macrophages>neutrophils | 20 h | >11 days | months |
| migrating keratinocytes | 2 days | >9 days | - |
| lipophages | 3 days | - | months |
| erythrophages | 3 days | - | months |
| siderophages/ haemosiderin | 3 days | - | months |
| granulation tissue | 3 days | - | months |
| complete re-epithelialisation | 5 days | >21 days | - |
| hematoidin | 8 days | - | months |
| lymphocyte-infiltrates | 8 days | - | months |
schema for the histological estimation of the age of open skin wounds and abrasions (Raekellio 1980)
| Survival period | Findings | ||||||||||
| <4 hours |
|
||||||||||
| 4-12 hours |
|
||||||||||
| 12- 48 hours |
|
||||||||||
| 2- 4 days |
|
||||||||||
| 4- 8 days |
|
||||||||||
| 8- 12 days |
|
||||||||||
| >12 days |
|
immunohistochemical parameters in age estimation of human skin wounds (Betz 2003)
| Antigen | Earliest appearance | Routine appearance | Latest appearance | |
| P-selectin | minutes | - | 7 h | |
| fibronectin | 10-20 min | >4 h | months | |
| E-selectin | 1 h | - | 17 days | |
| ICAM-1 | 1.5 h | - | 3.5 days | |
| fibroblast proliferation | 1.5 days | >6 days | - | |
| fibroblast apoptosis | 1-2 days | - | - | |
| tenascin | 2 days | >5 days | months | |
| collagen III | 2-3 days | >6 days | months | |
| collagen V | 3 days | >6 days | months | |
| collagen VI | 3 days | >6 days | months | |
| collagen I | 5 days | >6 days | months | |
| myofibroblasts | ||||
| laminin | 1.5 days | - | months | |
| HSPG | 1.5 days | - | months | |
| collagen IV | 4 days | - | months | |
| α actin | 5 days | - | months | |
| basement membrane | ||||
| bm-fragments | 4 days | >13 days | >21 days | |
| bm complete | 8 days | >21 days | - | |
| macrophage subtypes | ||||
| RM 3/1 | 7 days | - | - | |
| 25 F 9 | 11 days | - | - | |
| G 16/1 | 12 days | - | - | |
| complete staining of the epidermis for keratin 5 | 13 days | >23 days |
references
- Akasaka Y, Ono I, Yamashita T, Jimbow K, Ishii T (2004), 'Basic fibroblast growth factor promotes apoptosis and suppresses granulation tissue formation in acute incisional wounds', Journal of Pathology 203:710-720
- Betz P (1995), 'Immunohistochemical parameters for the age estimation of human skin wounds', Am Journal of Forensic Med Pathol 16(3):203-209
- Betz P (2003), 'Pathophysiology of wound healing', Ch. 8 in Payne-James J, Busuttil A, Smock W (Eds), 'Forensic Medicine - Clinical and Pathological Aspects', Greenwich Medical Media, London UK
- Cecchi R (2010), 'Estimating wound age: looking into the future', International Journal of Legal Medicine 124:523-536
- Fieguth A, Kleemann WJ, von Wasielewski R et al (1997), 'Influence of postmortem changes on immunohistochemical reactions in skin', Int J Legal Med 110:18-21
- Hernandez-Cueto C, Girela E, Sweet D (2000), 'Advances in the diagnosis of wound vitality: a review', Am Journal of Forensic Med Pathol 21(1):21-31
- Kondo T, Oshima T, Mori R et al (2002a), 'Immunohistochemical detection of chemokines in human skin wounds and its application to wound age determination', Int J Legal Med 116:87-91
- Kondo T, Tanaka J, Ishida Y et al (2002), 'Ubiquitin expression in skin wounds and its application to forensic wound age determination', Int J Legal Med 116:267-272
- McCausland IP, Dougherty R (1978), 'Histological ageing of bruises in lambs and calves', Australian Veterinary Journal 54:525-527
- Oehmichen M (2004), 'Vitality and time course of wounds', Forensic Science International 144:221-231
- Raekellio J (1980), 'Histological estimation of the age of injuries', Chapter 1 in: Perper JA and Wecht CH (Eds), 'Microscopic diagnosis in forensic pathology', Charles C Thomas, Springfield, Ill USA
- Suarez-Penaranda JM, Rodriguez-Calvo MS, Ortiz-Rey JA et al (2002), 'Demonstration of apoptosis in human skin injuries as an indicator of vital reaction', Int J Legal Med 116:109-112
- Takamiya M, Kiyoshi S, Yasuhiro A (2002), 'Immunohistochemical study of basic fibroblast growth factor and vascular endothelial growth factor expression for age determination of cutaneous wounds', Am Journal of Forensic Med Pathol 23(3):264-267
- Tarran S, Lanlois NEI, Dziewulski P, Sztynda T (2006), 'Using the inflammatory cell infiltrate to estimate the age of human burn wounds: a review and immunohistochemical study', Med Sci Law 46(2):115-126
